Introduction to Cpap Versus Bipap
If you have sleep apnea, COPD or another respiratory condition, you might be familiar with CPAP (Continuous Positive Airway Pressure) and BiPAP (Bilevel Positive Airway Pressure) machines. Both are highly effective noninvasive ventilation therapies that pump pressurized air to keep the airways open during sleep, but they work differently and cater to different needs.
In 2026, CPAP is still the gold standard treatment for most cases of obstructive sleep apnea (OSA), with BiPAP becoming more common in complex cases and individuals requiring higher pressure or who cannot tolerate CPAP. Knowing cpap versus bipap enables patients and caregivers to determine which is best for comfort, efficacy and long-term compliance.
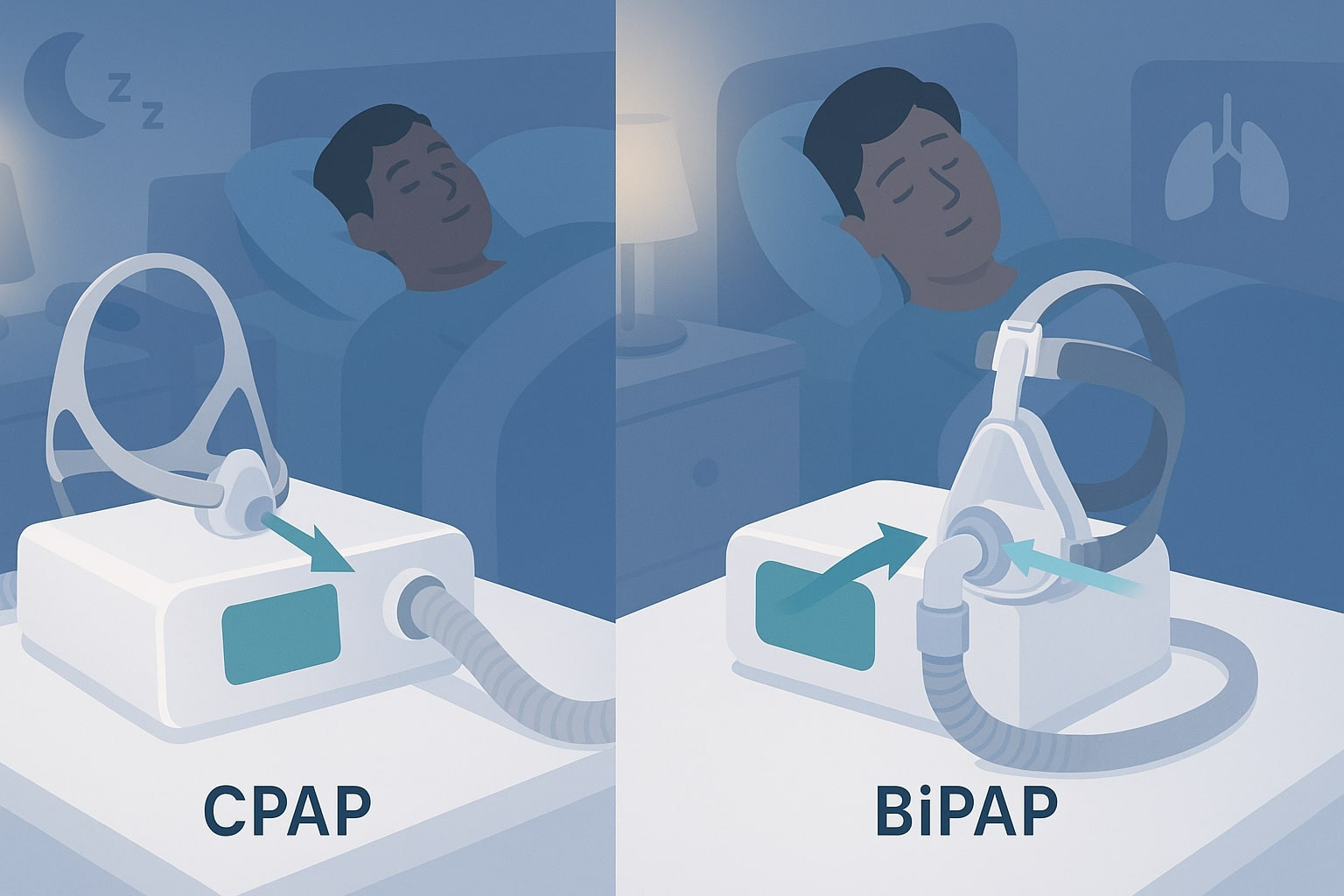
Here’s a side-to-side look at some of the machines, which are compact in size, with masks and interfaces frequently used in home settings:
Cpap Versus Bipap: Core Differences
The difference is in the way pressure is applied:
- CPAP — Delivers one single pressure all throughout the breath cycle – inhale and exhale. Pressures are usually set between 4–20 cm H₂O.
- BiPAP — This machine delivers two separate pressure points:
- More pressure when breathing in (IPAP – Inspiratory Positive Airway Pressure)
- During exhalation this pressure is reduced (EPAP – Expiratory Positive Airway Pressure)
Pressure range is often set between 4 and 30 cm H₂O, with the difference in pressure between IPAP and EPAP providing “pressure support” to facilitate breathing.
This bilevel decrease in the amount of work required to breathe out against pressure, and is why some find it preferable to use a BiPAP at high pressures.
Here are diagrams demonstrating the different flow patterns of “straight” single-pressure (CPAP) compared to bilevel technology (BiPAP), and both have clear pressurization waveforms so you can see at a glance what’s happening:
When Is CPAP Better? When Is BiPAP Better?
CPAP is the preferred initial therapy because it is simpler, has been studied more extensively and successfully treats most patients with OSA.
BiPAP shines when:
- Higher pressures (>15–20 cm H₂O) required — more easily tolerated because of lower exhale pressure.
- Patient discomfort (fighting to exhale/ air swallowing/aerophagia) with CPAP.
- Complicated conditions are present — CSA, mixed/complex apnea, COPD with hypercapnia, OHS, neuromuscular diseases or congestive heart failure.
- Better clearance of CO₂ is needed (BiPAP overcomes ventilation better).
It can be argued, based on clinical data, that the vast majority of patients with OSA will do well with CPAP; however, BiPAP has been shown to allow a more comfortable therapy for certain subpopulations (i.e., severe OSA + COPD or when attempts at CPAP fail).
Some common CPAP and BiPAP mask (nasal, full-face) examples featuring differences in fit and comfort:
Cpap Versus Bipap: Side-by-Side Comparison
| Feature | CPAP | BiPAP |
|---|---|---|
| Pressure Delivery | Single constant level | Two positions (upper inhale and lower exhale) |
| Best For | Most OSA cases | High-pressure needs, CSA, COPD, OHS |
| Comfort (Exhalation) | Might be harder feeling at high pressure | Easier to exhale |
| Cost (Machine) | Generally lower ($500–$1,500) | Higher ($1,700–$3,000+) |
| Insurance Coverage | Often first-line, easier approval | May require proof CPAP failed |
| Side Effects | Dry mouth/nose, mask leaks, aerophagia | Similar, often less aerophagia |
| Portability & Battery | Good, many travel-friendly | Similarly, some models supply longer battery |
Both rely on similar masks, hoses and humidifiers — comfort is often about fit, not the type of machine.
Here are graphic comparisons of CPAP vs BiPAP pressure settings and how the latter makes breathing easier:
CPAP vs BiPAP: Side Effects and Troubleshooting Problems
Side effects for both treatments are generally mild and can be treated:
- Dry mouth/nose (use heated humidification)
- Leakage or skin problems with mask (try another style/size)
- If claustrophobic or uncomfortable (start with ramp feature, ease adjustments)
- Aerophagia (air swallowing) — more pronounced with CPAP when pressures are increased
For some users, BiPAP tends to minimize aerophagia and exhalation discomfort leading to better compliance.
CPAP vs BiPAP Medicare Costs and Insurance
- CPAP — Less expensive out of pocket and most straightforward for insurance to cover as first-line OSA treatment.
- BiPAP — More expensive; generally must prove CPAP intolerance or specific diagnoses (CSA, COPD).
Plenty of vendors in Karachi and elsewhere sell them at rentals, or reconditioned machines or installments to make both accessible.
Cpap Versus Bipap FAQ
What’s the difference between CPAP and BiPAP?
CPAP applies one continuous pressure, whereas BiPAP delivers a higher inhalation pressure and then decreases it upon exhalation for more comfortable breathing.
Which is best for OSA?
CPAP therapy is generally the best and first option for uncomplicated OSA. BiPAP might be preferable if there is discomfort at higher pressures, or CPAP is not successful.
When is BiPAP better than CPAP?
BiPAP is commonly used for the treatment of central/complex sleep apnea, COPD with hypercapnia, obesity hypoventilation syndrome (OHS), and patients who are unable to tolerate CPAP.
Does CPAP or BiPAP have different side effects?
Same (dryness, leaks, irritation), but BiPAP usually results in less aerophagia and difficulty exhaling due to the lower exhale pressure.
Which is costlier — CPAP or BiPAP?
BiPAP machines are usually more expensive (more complicated), and insurance might cover either with good documentation.
Can I go from CPAP to BiPAP if I’m not getting relief on a CPAP?
Yes — many people switch successfully after consulting a sleep specialist. A titration trial, or study, can find out.
Can you use a CPAP mask with a BiPAP machine?
Many, if not most, masks are compatible with both types of machines, though high-pressure users looking for the right fit might require full-face or specialty masks to get a good seal.
How do I know which one to get?
A sleep study (polysomnography) and discussion with pulmonologist or sleep specialist will determine what option is best for you based on your diagnosis, pressure needs, and tolerance.
Which is better CPAP or BiPAP? The choice between CPAP and BiPAP totally depends on your condition, pressure required (Your Doctor / Sleep Specialist should recommend pressure), how do you find it more comfortable, etc. Both are life-altering for improved sleep and health — see a pro to get personalized tips in 2026!